* By GEOFFREY KABAT
This week’s news that the World Health Organization has classified processed meats and red meat as human carcinogens has once again drawn attention to how difficult it is to convey to the public the state of scientific knowledge on these sorts of questions.
It also points out just how skewed and confusing is WHO’s scheme for classifying carcinogens.
Other recent pronouncements by WHO’s International Agency for Research on Cancer that have perplexed both scientists and the public have involved the herbicide glyphosate, better known as Roundup, and cellphone “radiation.”
IARC reviews all available scientific evidence on a particular chemical, biological, or physical agent and classifies potential carcinogenic hazards according to the following scheme:
Group 1: Carcinogenic to humans
Group 2A: Probably carcinogenic to humans
Group 2B: Possibly carcinogenic to humans
Group 3: Not classifiable as to carcinogenicity
Group 4: Probably not carcinogenic
Of the nearly 1,000 substances IARC has assessed over the years, only one has been placed in Group 4. Thus, it appears that in practice IARC’s scheme disposes against declaring that an agent is unlikely to be a carcinogenic hazard.
The confusion and alarm set off by the processed meats announcement stems from the inclusion of this hazard in Group 1, putting it in the company of cigarette smoke, alcohol, asbestos, sunlight, and certain viruses. However, the Group 1 classification does not mean that the hazard associated with consuming hot dogs, sausages, or bacon is comparable to smoking a pack a day. It merely reflects IARC’s judgment that the scientific evidence that consumption of these foods can cause certain cancers is strong, but it says nothing about the magnitude of the risk or what level of consumption of these foods is dangerous. It is clear that we are talking about a much weaker and subtler risk than that associated with smoking.
Beyond the misunderstandings and confusion caused by the broadcasting of this judgment regarding processed meats, other assessments by the IARC do not square with the actual scientific evidence. This is perhaps nowhere more apparent than in the agency’s assessment of coffee.
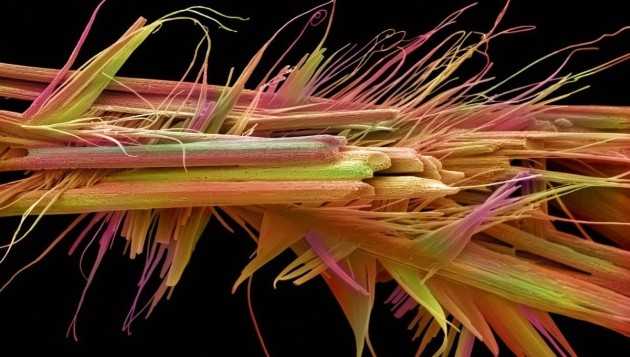
In 1991 the IARC classified coffee as “possibly carcinogenic to the human urinary bladder” (Group 2B). This conclusion was arrived at after reviewing the limited evidence available at that time. IARC noted that the data “are consistent with a weak positive relationship between coffee consumption and the occurrence of bladder cancer, but the possibility that this is due to bias or confounding cannot be excluded.” IARC did not find convincing evidence for an association of coffee with other types of cancer.
As an object of scientific study, coffee is different from Roundup, cellphone radiation, or the many chemicals IARC assesses. This is because coffee drinking is a habitual behavior that is relatively stable, and people can tell researchers with a fair degree of accuracy how long they’ve been drinking coffee and how many cups they usually consume per day. This means that exposure data should be of considerably higher quality than it is in studies of trace chemicals in the body, reports of cellphone use, or of how much dietary fat an individual has consumed over a period of decades.
Furthermore, coffee is consumed by a large proportion of the population in Western countries and, yet, importantly, there is a proportion of the population that does not consume it. Among consumers, there is a wide range in the number of cups of coffee consumed. Thus, coffee consumption is amenable to study with respect to an individual’s exposure (present or absent) as well as the dose among those who drink coffee. This means that, if coffee drinking were in fact associated with cancer, we would stand an excellent chance of detecting it.
The possible link between coffee-drinking and cancer has been studied since 1971. Most studies conducted in the 1970s through the 1990s were case-control studies. This type of study enrolls patients with the disease of interest (say, bladder cancer) and compares their exposures to those of “controls,” who may either be patients hospitalized with other diseases or healthy persons. Theoretically, the controls are comparable to the cases except for the absence of the disease of interest.
Case-control studies are subject to recall bias because people with a serious illness are likely to report their past exposures differently from controls, due to their desire to explain why they developed their disease.
Early studies focused on cancer of the bladder and kidney and showed inconsistent associations with coffee consumption. The ambiguous results of these studies stimulated further research, and many studies were undertaken examining a range of different types of cancer.
In the past two decades, results from cohort studies have appeared. In this type of study, a large population is enrolled in a study, and information about the participants’ health and behaviors is collected at the time the study begins. The cohort is then followed for a number of years and monitored for the development of disease. This type of study design is not susceptible to the problem of recall bias, since information about exposure is collected prior to the development of disease.
As of 2010, more than 500 studies of the association of coffee intake with various types of cancer have been published. The results of these studies have been summarized in meta-analyses to determine whether there is a consistent association of coffee drinking and cancer of a specific type.
What these meta-analyses and qualitative reviews show is that coffee drinking is associated with reduced risk of several cancers, including endometrial, colorectal, liver, and postmenopausal breast cancer. In the case of liver cancer, coffee drinkers have roughly a 50 percent reduction in risk. For other cancers, including bladder, kidney, prostate, pancreas, and ovary, there is no consistent evidence of an association.
IARC’s initial classification of coffee as a possible carcinogen and its failure to update its assessment in the light of the extensive evidence that has accumulated over the past 25 years highlight a larger problem with the agency’s scheme for classifying carcinogens.
The IARC gives greater weight to positive results than to negative results, even when the latter are from higher-caliber studies.
It is easy to see how this mind-set can lead to an upward shift in the classification of a given agent. And this explains why, of all the nearly 1,000 agents IARC has assessed, exactly one has been categorized as “not likely to cause cancer.”
As the biostatistician Donald Berry commented in 2011, at the time IARC placed cellphone radiation in Group 2B, “anything is a possible carcinogen.”
Coffee is the one of the most widely consumed beverages in the world and one of the most extensively studied components of diet. If we can’t declare coffee to be “unlikely to cause cancer,” what does that say about our ability to assess much more difficult and subtle risks?